Understanding Paroxysmal Hemicrania (PH): Symptoms, Treatment, and Differentiation from Other Headaches
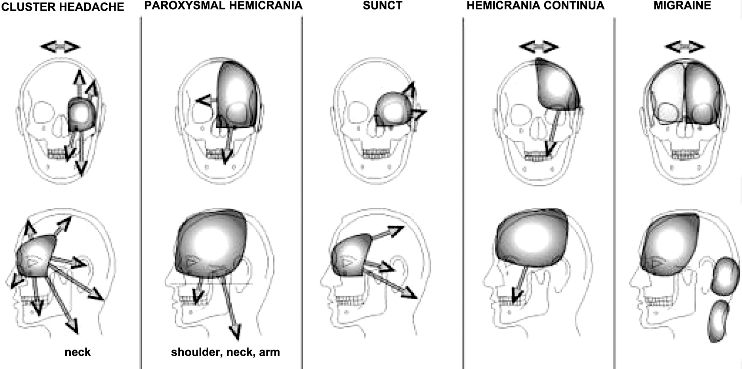
Paroxysmal hemicrania (PH) stands out as a distinct type of headache marked by intense, one-sided throbbing or piercing pain, localized in the ocular, temporal, or frontal areas, lasting anywhere from 2 to 30 minutes. Notably, PH patients also experience accompanying cranial autonomic manifestations such as tearing, reddening of the eye, nasal congestion, runny nose, sweating across the forehead and face, pinpoint pupils, and drooping eyelids during these headache episodes. With attacks recurring frequently throughout the day, ranging from 5 to 40 times, PH typically shows a positive response to indomethacin therapy. These defining characteristics set PH apart from other headache types, particularly concerning the unilateral pain pattern, associated autonomic symptoms, attack frequency, and the specific effectiveness of indomethacin treatment.
Exploring Non-Invasive Vagus Nerve Stimulation (nVNS) as a Promising Treatment for Paroxysmal Hemicrania (PH) and Other Trigeminal Autonomic Cephalalgias (TACs)
A new research paper delves into the potential of non-invasive vagus nerve stimulation (nVNS) as an alternative therapeutic approach for patients grappling with paroxysmal hemicrania (PH) and unable to withstand conventional treatments like indomethacin.
Through a compelling case study involving a female patient with PH and sleep apnoea, the study unveils encouraging results: temporary relief from headaches through positive airway pressure (PAP) treatments and a favorable response to transauricular vagus nerve stimulation (ta-VNS).
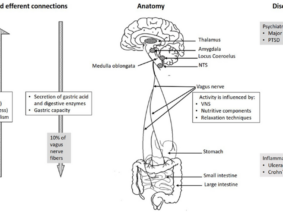
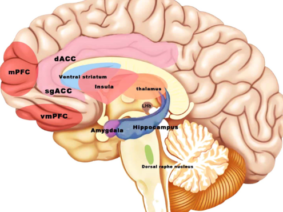
The authors meticulously assessed the impact of ta-VNS by scrutinizing the patient’s sympathetic skin responses using an electromyography (EMG) device. Their findings hint at potential autonomic system implications in PH cases, indicating the prospect of achieving autonomic system modulation with nVNS. While emphasizing the necessity for broader case studies to delve deeper into these realms, the paper highlights the promising outcomes of ta-VNS in PH treatment and its potential broader implications for trigeminal autonomic cephalalgias (TACs). These primary headache disorders share common clinical features like unilateral pain, autonomic symptoms, and brief attack durations.
Research indicates the positive impact of ta-VNS in chronic cluster headache, another type of TAC, by decreasing attack frequency and intensity. However, the potential applications of ta-VNS for other TACs such as short-lasting unilateral neuralgiform headache attacks (SUNHAs) and hemicrania continua remain largely unexplored.
In summary, this study sheds light on the potential of nVNS in PH management and the assessment of sympathetic skin responses as an evaluative tool for this treatment’s effectiveness.
This non-invasive treatment avenue offers hope for individuals grappling with these uncommon headache types and unable to tolerate traditional treatments. However, comprehensive research is essential to ascertain the complete effectiveness of ta-VNS in managing TACs
References:
Benoliel R. Trigeminal autonomic cephalgias. British Journal of Pain. 2012;6(3):106-123. doi:10.1177/2049463712456355